Also Offering Dry Eye Treatment for Johns Creek & Dunwoody

But while everyone exhibits similar symptoms of Dry Eye Syndrome, also called DES, Dry Eye, or Ocular Surface Disease (OSD), the causes can vary so widely that an effective treatment can be difficult to find.
So, does dry eye go away? The simple answer is no. Dry eye won’t go away by itself. There are high-quality, effective treatments used to alleviate the itching and burning of dry eye, however, and your eye care provider can help you find the solution that’s right for you.
At Atlanta Vision Institute, we offer a range of solutions aimed at reducing the symptoms of chronic dry eye, helping you get you the relief you deserve.
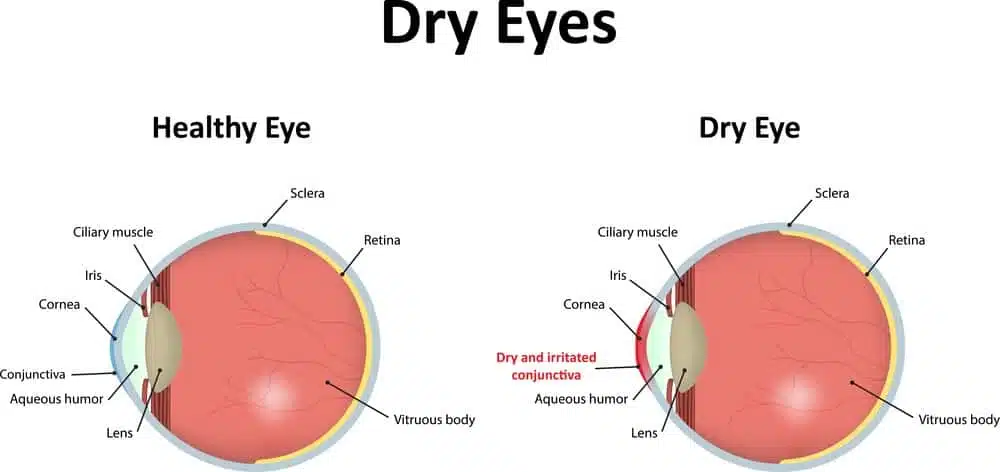
What is Dry Eye and What Causes It?
Dry eye, or Ocular Surface Disease, is diagnosed any time a patient reports suffering from chronic dryness, redness, itching, burning or other irritation in the eye. Because the causes can vary so much, “dry eye” ends up serving as a blanket term for the symptoms rather than a documented condition.
Little is known about the causes of the disorder but dry eyes often have to do with a dysfunction of the Meibomian gland (the few dozen tiny glands in your eyes that produce tears). Tear glands support total eye lubrication, so Meibomian Gland Dysfunction, or MGD, is a common cause of dry eyes.
Dry eyes are common in people age 50 or older, as well as among those who spend most of their time in air-conditioned or heated rooms or looking at screens for long periods of time. Because of the increase in occupations that involve computer screens — the American Academy of Ophthalmology (AAO) estimates that the average worker spends 1,700 hours in front of a screen per year — experts worry about the lasting effects on vision in addition to a significant increase in cases of dry eye disorder.
People on medications such as antidepressants, contact lenses wearers or those diagnosed with lupus also report dry eyes at a higher rate than the average American.
Another common cause of dry eye is blepharitis, inflammation of the eyelids, commonly caused by poor eyelid hygiene or the presence of Demodex, tiny organisms that inhabit the hair follicles and oil glands found around the eye.
How I Can Prevent Dry Eye
The best treatment for dry eyes is self-care and prevention. Make sure you keep your eyes clean and take breaks to rest your eyes when using a computer screen. A humidifier can greatly alleviate the itchiness and soreness of dry eyes and warm compresses can provide additional relief. For mild cases of dry eyes due to situational causes (schoolwork, reading or office work), doctors recommend artificial tears or other lubricating eye drops.
These lifestyle changes are among a range of methods that can be used to make dry eye go away, but they may only be temporary. It’s likely, for example, that if you move from a dry climate to a humid one, your symptoms may be alleviated, but this doesn’t mean you won’t have to worry about these symptoms should you move back to a dry climate again.
Permanent Dry Eye Relief
Dry eye syndrome can be frustrating to live with. When you’re unable to pinpoint the cause of your symptoms, it can be difficult to solve, which is what many patients with itchy, irritated eyes have to go through.
This is why it’s important that your eye doctors have a variety of treatments: whether you’re suffering from itchy eyelids, blurry vision, or some other symptom of OSD, you may have to try a few different potential solutions before you can get the relief you need.
For severe dry eyes caused by an underlying Meibomian Gland Dysfunction, however, the solutions mentioned may provide little to no relief.
Prescription Medications for Dry Eye Syndrome
Currently, there are only two FDA-approved drugs for the treatment of dry eyes.
- Restasis is a type of eye drop which includes an agent that reduces the inflammation associated with dry eye syndrome and encourages your body to produce more natural tears to hydrate your eyes. To be effective, the eye drops need to be used for a minimum of 90 days.
- Lifitegrast (also known under its trade name Xiidra) is another FDA-approved treatment. Like Restasis, it aims to reduce the inflammation all while lubricating your eyes. Both drugs come with side effects such as burning during the initial use, eye irritation and altered taste sensation (reported in 5-25% of patients). Both Xiidra and Restasis provide relief to the dry eye syndrome’s symptoms in around 20-30% of patients and need to be taken regularly.
IPL Treatment for Dry Eye
Recently, another long-term treatment for dry eye syndrome caused by Meibomian Gland dysfunction has been introduced to physicians:
IPL, or Intense Pulsed Light Treatment, focuses a strategic level of light pulses in the 500-800nm wavelength range that penetrates the skin under the eye and targets the malfunctioning Meibomian gland.
This causes an increase in the temperature and thrombosis of the blood vessels, which in turn can break up the blockages in the tear glands and improve the healthy tear production.
Research is still being done on the effectiveness of IPL, but a preliminary study from 2015 found objective improvement in 87% of patients. IPL treatment only requires 3-4 eight-minute sessions and the effects can last for as long as one year.
Frequently Asked Questions About Dry Eye Disease
If I have dry eye, does it mean that my eyes are not producing enough tears?
Possibly. Or, you may be producing tears but the tears are of poor quality and therefore unable to sufficiently moisturize your eyes.
What is meibomian gland dysfunction?
Most cases of dry eye are caused by meibomian gland dysfunction (MGD).
The meibomian glands are tiny glands in the eyelids that secrete the oily layer of the tear film. The oil helps tears “stick” to the ocular surface and keep the eyes lubricated. Sometimes the meibomian glands become blocked with hardened or thickened oil secretions. Without sufficient oil, tears evaporate too rapidly off the surface of the eyes. As a result, the eyes can become dry, irritated and itchy.
Treatment for MGD involves melting and clearing the thickened secretions to restart the normal flow of oil to the tear film. Dr. Ashraf can also treat inflamed blood vessels around the meibomian glands that interfere with normal gland function.
How is dry eye disease diagnosed?
Dry eye diagnosis involves a comprehensive eye exam and an evaluation of the volume and quality of your tears. Dr. Ashraf will also ask you about your symptoms and review your history of overall health and eye health to look for any factors that could cause or contribute to dry eye disease.
Can I wear contacts if I have symptoms of dry eye disease?
In some cases, contact lens use may exacerbate the symptoms of dry eye disease.
If you normally wear contacts but suffer the uncomfortable symptoms of dry eye, talk to Dr. Ashraf about your options. He may suggest another type or brand of contacts that are less likely to aggravate your eyes.
Who should not use Restasis and Lifitegrast (Xiidra) drops?
You should not use either of these medications if you are allergic to any of the ingredients. Talk to Dr. Ashraf to determine whether you can benefit from using these drops, or whether another medical or surgical therapy is more appropriate.
Who is most likely to get dry eye disease?
Women — especially those experiencing hormonal changes due to pregnancy, menopause or oral contraceptive use — are more likely to develop dry eye. Dry eye is also common among older adults, as tear production naturally slows around the age of 50.
Other factors that can increase the risk of dry eyes include the following:
- Spending prolonged periods of time in front of digital screens
- Use of certain medications (e.g., antihistamines, decongestants)
- History of certain medical conditions (e.g., rheumatoid arthritis, diabetes, thyroid disease)
How does IPL improve the symptoms of dry eye?
IPL addresses the root cause of some dry eye cases instead of simply alleviating the symptoms. The treatment uses light energy to target abnormal blood vessels causing inflammation around the eyelids that interferes with meibomian gland dysfunction. This enables the glands to resume secreting oils into the tear film so the tears do not evaporate prematurely.
Can dry eye disease be cured?
Unfortunately dry eye is a chronic condition and there is no permanent cure. With Dr. Ashraf’s experience and knowledge, he can provide treatment solutions to manage your symptoms.
Learn More About Dry Eye Treatment
Since dry eye is such a complicated disorder, not every solution will work to treat the symptoms, which is why it’s important to trust your eyes to a team with experience. The eye care experts you trust with your eyes will carry out tests and examinations to find the source of your chronic irritated eyes, which should show them which solutions will make the most impact.
Atlanta Vision prides ourselves as one of the first providers to incorporate new technology in the battle against dry eyes and other areas of our practice. From IPL to help dry eye go away to minimally-invasive refractive surgery, Atlanta Vision Institute is your source of high-quality eye care.
Please Take Our LASIK or Cataract Surgery Quiz
Take our vision quiz to find out if you qualify for LASIK or cataract surgery!